Saturday, December 27, 2014
The Mix has moved
Stay up to date with the latest stories and insights from UAB research at our new location, www.uab.edu/mix.


Monday, December 22, 2014
Change agent: Creating new scans to track brain diseases
Seven weeks after weight-loss surgery, a group of women have seen significant changes in their body shapes and sizes. They’re each down 20 to 30 pounds, but that’s not the only change their bodies are going through.
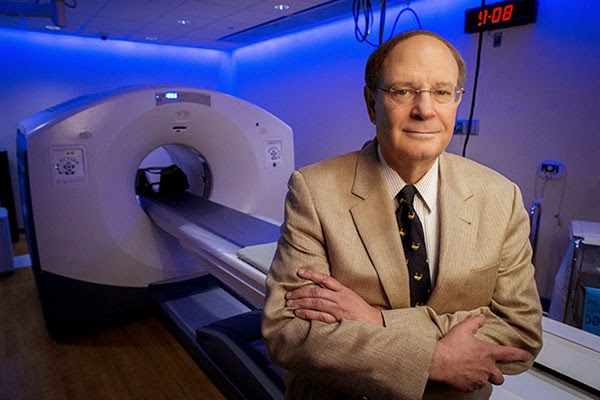
The women’s weight loss is caused by a change in appetite, which results from changes in brain function, explains UAB neuroradiologist Robert Kessler, M.D. (pictured above in UAB's Advanced Imaging Facility). On positron emission tomography (PET) scans, Kessler can see an obvious transformation in the women’s brains, particularly in dopamine neurotransmission.
Using a specialized brain PET scan that he has developed, Kessler can visualize levels of dopamine receptors — molecules that help transmit the brain’s messages of motivation and reward. Before surgery, the women had increased levels of the receptors, which appear on the PET scans as glowing white patches throughout the brain. But after their surgeries, these changes have faded; the women’s brains exhibit a more balanced map of dopamine receptors. In real-world terms, Kessler thinks, these tempered receptor levels reflect a shift to a more normal reward perception, helping the women control their appetites after surgery.
Obesity — and the drive to overeat — isn’t the only pathology that Kessler can see when he peers into people’s brains with a PET scan. During the past 30 years, he has helped illuminate changes to the brain that might underlie schizophrenia, drug addiction, depression and dementia, among other disorders. By looking at a person’s brain PET scan and carefully measuring the levels of neurotransmitter function, Kessler can tell whether someone is more prone to taking risks than average, whether they’re more of a “slacker” or a “go-getter,” and whether or not they have “the ability to experience rewarding stimuli in a normal manner or if they have lost that ability,” he said.
Kessler, who joined the UAB faculty in 2013 as director of neurochemical brain imaging and PET neurotracer development in the Department of Radiology, says these specialized PET scans are paving the way toward a new level of understanding of brain diseases.
“At a very basic scientific level, there’s no other technology that can look at the human brain and inform you about specific molecules and receptors,” Kessler said. At UAB, he’s taking advantage of the university’s TR24 cyclotron — the largest at any U.S. academic medical center — to develop new PET scans. And he has launched collaborations with UAB researchers across the psychiatric and neurological sciences to help them apply his techniques to even more questions.
In 1977, Kessler joined a lab at the National Institutes of Health just as this was changing. One of his mentors there became the first to use a PET scan to visualize the activity of the brain. The earliest scans, rather than pinpointing specific receptors as Kessler does now, were designed to simply show which cells in the brain were undergoing metabolism — a sign of activity — at any given moment.
But the basic idea has been the same for more than three decades now: A patient gets an injection of a radioactive tracer into their bloodstream. Depending on the design of the tracer, it accumulates in particular organs or cells of the body. Then, a PET machine is used to measure the location of the accumulated radioactivity.
“It quickly became clear to me that PET was going to become an important tool for understanding the brain,” Kessler said. “And we began to use it to look at everything from brain tumors and schizophrenia to aging and dementia.”
As Kessler immersed himself in the new technology, first at NIH and then at Vanderbilt University, he helped develop new tracers that would pave the way for the rest of his career: 18F-Fallypride, and later 18F-FPEB. Rather than building up in all metabolizing brain cells, these radioactive molecules bind specifically to dopamine and glutamate receptors.
Among the first questions Kessler asked with 18F-Fallypride was ‘What are the effects of antipsychotic drugs on the brains of patients with schizophrenia?’ A new class of antipsychotic drug had recently been developed; the drugs had fewer side-effects than older versions, but researchers didn’t know why. Kessler and his collaborators discovered that the new drugs targeted different areas of the brain than the old drugs, offering not only an explanation for the differences, but a way to test future drugs for their efficacy.
Dopamine had also already become known as a chemical that mediates reward-seeking behavior and pleasure. So Kessler’s lab began to look at how levels of the dopamine receptor and the effects of dopamine release on dopamine receptors might relate to drug abuse, impulse control, addiction and the ability to feel pleasure.
“People who are depressed lose their ability to enjoy rewards and experience the pleasures of life; people who are addicted have very distorted reward functions where they crave just one reward,” Kessler said. “We showed that dopamine plays a key role in all of these.”
One of the ongoing challenges in the field, Kessler says, is developing new tracers. With UAB’s new cyclotron, Kessler says he has the tools at his fingertips to continue developing and perfecting tracers that bind to different receptors in the brain. He’s already begun work with the neurotransmitter glutamate; like dopamine, glutamate can be studied through PET tracers that bind to glutamate receptors. And glutamate is thought to have roles in autism, Huntington’s disease, Parkinson’s and anxiety disorders, among other things.
This fall, Kessler launched a study examining glutamate receptors in the brains of addicts as they voluntarily withdraw from methamphetamine. The findings — if they show key differences from normal brains — could lead to new drugs to help meth addicts quit their addiction. Studies on Parkinson’s, depression and Alzheimer’s disease are also in the works with UAB collaborators.
Although “this is a tough area to work in for many reasons,” Kessler said — from the vagaries of chemical half-lives to the sheer complexity of the brain itself — he wouldn’t have it any other way. “You just can’t get this kind of information anywhere else.”
The women’s weight loss is caused by a change in appetite, which results from changes in brain function, explains UAB neuroradiologist Robert Kessler, M.D. (pictured above in UAB's Advanced Imaging Facility). On positron emission tomography (PET) scans, Kessler can see an obvious transformation in the women’s brains, particularly in dopamine neurotransmission.
Using a specialized brain PET scan that he has developed, Kessler can visualize levels of dopamine receptors — molecules that help transmit the brain’s messages of motivation and reward. Before surgery, the women had increased levels of the receptors, which appear on the PET scans as glowing white patches throughout the brain. But after their surgeries, these changes have faded; the women’s brains exhibit a more balanced map of dopamine receptors. In real-world terms, Kessler thinks, these tempered receptor levels reflect a shift to a more normal reward perception, helping the women control their appetites after surgery.
Obesity — and the drive to overeat — isn’t the only pathology that Kessler can see when he peers into people’s brains with a PET scan. During the past 30 years, he has helped illuminate changes to the brain that might underlie schizophrenia, drug addiction, depression and dementia, among other disorders. By looking at a person’s brain PET scan and carefully measuring the levels of neurotransmitter function, Kessler can tell whether someone is more prone to taking risks than average, whether they’re more of a “slacker” or a “go-getter,” and whether or not they have “the ability to experience rewarding stimuli in a normal manner or if they have lost that ability,” he said.
| Find out how a cyclotron works, and what makes UAB’s new cyclotron unique among U.S. academic medical centers, in the video above and in this feature from UAB Magazine. |
“At a very basic scientific level, there’s no other technology that can look at the human brain and inform you about specific molecules and receptors,” Kessler said. At UAB, he’s taking advantage of the university’s TR24 cyclotron — the largest at any U.S. academic medical center — to develop new PET scans. And he has launched collaborations with UAB researchers across the psychiatric and neurological sciences to help them apply his techniques to even more questions.
Focusing on Receptors
As a medical student, resident and fellow in the 1970s, Kessler first became interested in the human brain at a time that clinicians had few methods to visualize the organ. Surgeons could physically see the outer layers of the brain when they opened the skull for an operation, or pathologists could dissect an autopsied brain; but viewing the activity — in a living human — of the molecules that make up the brain’s electrical pathways wasn’t possible.In 1977, Kessler joined a lab at the National Institutes of Health just as this was changing. One of his mentors there became the first to use a PET scan to visualize the activity of the brain. The earliest scans, rather than pinpointing specific receptors as Kessler does now, were designed to simply show which cells in the brain were undergoing metabolism — a sign of activity — at any given moment.
But the basic idea has been the same for more than three decades now: A patient gets an injection of a radioactive tracer into their bloodstream. Depending on the design of the tracer, it accumulates in particular organs or cells of the body. Then, a PET machine is used to measure the location of the accumulated radioactivity.
“It quickly became clear to me that PET was going to become an important tool for understanding the brain,” Kessler said. “And we began to use it to look at everything from brain tumors and schizophrenia to aging and dementia.”
As Kessler immersed himself in the new technology, first at NIH and then at Vanderbilt University, he helped develop new tracers that would pave the way for the rest of his career: 18F-Fallypride, and later 18F-FPEB. Rather than building up in all metabolizing brain cells, these radioactive molecules bind specifically to dopamine and glutamate receptors.
Among the first questions Kessler asked with 18F-Fallypride was ‘What are the effects of antipsychotic drugs on the brains of patients with schizophrenia?’ A new class of antipsychotic drug had recently been developed; the drugs had fewer side-effects than older versions, but researchers didn’t know why. Kessler and his collaborators discovered that the new drugs targeted different areas of the brain than the old drugs, offering not only an explanation for the differences, but a way to test future drugs for their efficacy.
Dopamine had also already become known as a chemical that mediates reward-seeking behavior and pleasure. So Kessler’s lab began to look at how levels of the dopamine receptor and the effects of dopamine release on dopamine receptors might relate to drug abuse, impulse control, addiction and the ability to feel pleasure.
“People who are depressed lose their ability to enjoy rewards and experience the pleasures of life; people who are addicted have very distorted reward functions where they crave just one reward,” Kessler said. “We showed that dopamine plays a key role in all of these.”
 |
| These are 18F-Fallypride PET images of dopamine D2 type receptors, averaged across several normal subjects. There are high levels of these receptors (red color) in deep brain structures and lower levels in the cortex. These include the basal ganglia and thalamus (A), amygdala and temporal cortex (B), and substantia nigra (C). These regions are concerned with movement, emotion and cognition. |
The Future of Brain PET
PET scans offer the most direct way to observe what happens at a molecular level in the brain when someone develops, or recovers from, a psychiatric disorder or addiction, Kessler says. Drug developers and pharmaceutical companies now use PET scans to fine-tune prospective new treatments, he notes. If they know they need to lower the number of dopamine receptors in one area of the brain, for instance, they can use PET scans to determine which drugs, and drug dosages, effectively achieve this.One of the ongoing challenges in the field, Kessler says, is developing new tracers. With UAB’s new cyclotron, Kessler says he has the tools at his fingertips to continue developing and perfecting tracers that bind to different receptors in the brain. He’s already begun work with the neurotransmitter glutamate; like dopamine, glutamate can be studied through PET tracers that bind to glutamate receptors. And glutamate is thought to have roles in autism, Huntington’s disease, Parkinson’s and anxiety disorders, among other things.
This fall, Kessler launched a study examining glutamate receptors in the brains of addicts as they voluntarily withdraw from methamphetamine. The findings — if they show key differences from normal brains — could lead to new drugs to help meth addicts quit their addiction. Studies on Parkinson’s, depression and Alzheimer’s disease are also in the works with UAB collaborators.
Although “this is a tough area to work in for many reasons,” Kessler said — from the vagaries of chemical half-lives to the sheer complexity of the brain itself — he wouldn’t have it any other way. “You just can’t get this kind of information anywhere else.”
Monday, December 15, 2014
Equations against cancer: Using math to predict a tumor's path
Hassan Fathallah-Shaykh, M.D., Ph.D., believes that math can transform medicine, and he has the numbers to prove it.
In the clinic, this UAB neurologist specializes in treating brain tumors. In his lab at the Comprehensive Cancer Center, Fathallah-Shaykh, who is also a professor of mathematics at UAB, wields equations as well as petri dishes. His mathematical models of cancer behavior are offering new insights on tumor growth. Eventually, they could be used to personalize treatment based on the unique characteristics of each patient’s cancer cells and anatomy.
Fathallah-Shaykh is one of a growing number of researchers worldwide exploring the field of mathematical biology, which “uses mathematical tools to generate models of biological problems,” he said. Building mathematical models based on the current understanding of a disease, for example, allows researchers to “test whether the assumptions are accurate,” Fathallah-Shaykh said.
 |
| Hassan Fathallah-Shaykh |
Model Behavior
Working with colleagues at the University of Bordeaux, and UAB graduate student Elizabeth Scribner, Fathallah-Shaykh has created an elegant model of the aggressive brain cancer glioblastoma multiforme (GBM). It produces simulations on the scale of clinical MRI scans, so that its predictions can be tested directly against patient data. In a paper published on Dec. 15 in PLOS ONE, the researchers demonstrated that their model can reproduce the typical GBM growth patterns seen on patient scans. They also revealed its value as a research tool.The model predicted a previously unknown pattern of tumor growth in patients with recurrent GBM treated with the anti-angiogenesis drug bevacizumab. This growth, powered by a cycle of proliferation and brain invasion, is characterized by an expanding area of invasive cells and dead cells known as necrosis, the researchers say. A subsequent search of 70 patient MRI scans by the researchers turned up the same pattern in 11 cases.
“We hope to tailor radiation therapy, chemotherapy and other treatments based on a personalized model of a patient’s tumor.”
That pattern explains the disappointing results of recent Phase III clinical trials of anti-angiogenesis therapies against GBM, the researchers say. Anti-angiogenesis drugs attempt to kill tumors by preventing them from growing new blood vessels. But the model demonstrated how GBM cells can flee from the oxygen-depleted treatment area — and quickly begin expanding again as soon as therapy stops or the tumor becomes resistant to the drugs. (For more on the model and these findings, see “SimTumor,” below.)
“We’ve shown that we can predict new insights on cancer behavior,” Fathallah-Shaykh said. The results have already spurred Fathallah-Shaykh to pursue new therapies in his lab to limit tumor mobility. Ultimately, the researchers hope to use their model to personalize therapy to the unique characteristics of a patient’s tumor. They could do that by analyzing the existing growth pattern of a tumor and building that into the model’s parameters. Then they could simulate its future behavior on a virtual MRI slice that reproduces the unique anatomy of the patient’s brain. “We hope to tailor radiation therapy, chemotherapy and other treatments based on a personalized model of a patient’s tumor,” said Fathallah-Shaykh.
Advancing Mathematical Biology ResearchThis spring, Fathallah-Shaykh helped organize a symposium on the topic as part of the College of Arts and Sciences’ Interdisciplinary Innovation Forum series. The meeting attracted some of the mathematical biology’s most famous names. Meanwhile, he is helping to attract new talent to the discipline by teaching undergraduate and graduate courses on Mathematical Biology in the math department. “It is quite clear that the next great advances in medicine cannot happen without math,” Fathallah-Shaykh said. “These are exciting times.” |
From Flies to Colon Cancer
Since he joined the UAB faculty in 2008, Fathallah-Shaykh has been developing ever more advanced models to predict the behavior of biological networks. He began by building a model of the molecular clock in a fruit fly’s brain. Despite the fly’s tiny size, it’s a challenging puzzle. The clock is a tangled web of positive and negative feedback loops, with five different genes producing proteins that inhibit and activate one another (as well as themselves, in some cases) in a regular cycle.First, Fathallah-Shaykh and his collaborators “showed we can replicate everything the clock is known to do,” he said. Then they proved it was a useful research tool, answering a perplexing question about the fruit-fly gene Clockwork Orange that had stumped biologists for years.
The researchers next adapted their model to track the developing neural networks in fruit-fly embryos. To do this, they utilized the Kalman filter, a mathematical technique to analyze and predict changes that helps track planes in flight. Now, “we’re using the model to study molecular networks in colon cancer,” Fathallah-Shaykh said.
Coping with an Information Explosion
Fathallah-Shaykh has always been fascinated with math. “It’s like a symphony; it’s beautiful,” he said. “But it’s also very applicable.” He cemented the connection between medicine and math as a neurologist at Rush University Medical Center in Chicago when he enrolled in a doctoral program in mathematics at the nearby University of Illinois–Chicago. “I would go to class in between patients,” he said.Math is essential to making progress against the toughest questions in medicine, Fathallah-Shaykh contends. To illustrate the problems that researchers face, he points to a chart of all the known molecular pathways involved in Alzheimer’s disease. It’s a mass of interlocking loops and tangles that fills an entire page. Researchers specialize in tiny sections of this wiring diagram, but understanding how it all works together is another problem entirely. Even worse, these networks are intertwined in such a way that multiple paths can lead to the same destination. That may help explain why treatments that work beautifully in isolated cell lines in a lab so often fail when they encounter the complex networks of the body.
There’s another wrinkle. “Cells migrate, they communicate, they interact with one another over time,” said Fathallah-Shaykh. The waves of mutations, which are a hallmark of cancer, make the problem particularly complex, he noted. “Whole pathways are deleted and new connections start turning up.” It’s a perfect example of a nonlinear dynamic system, like the weather or the stock market, in which slight changes in one parameter can lead to wildly diverging outcomes.
The good news, said Fathallah-Shaykh, is that “mathematics has very rich tools” to model just these types of systems, as he has demonstrated with his cancer simulations. But this work has another exciting element for Fathallah-Shaykh as a mathematician: It opens new horizons in math theory. “Equations have already been developed from biological problems,” he said, “and there is very strong evidence that they will produce spectacular advances in mathematics.”
SimTumor
At the heart of Hassan Fathallah-Shaykh’s new mathematical model of glioblastoma multiforme (GBM) are 10 partial differential equations. Here’s how it works — and what it has revealed about GBM behavior.
Formula 10
Equations track each of four different cell types, with unique rules of behavior.
Proliferative GBM cells (P), which make up the bulk of the tumor, divide but don’t move.
Invasive GBM cells (I), found on the fringes of the tumor, move but don’t divide.
Healthy brain cells (B) neither divide nor move, although they are displaced by the growing tumor.
Cells in the center of the tumor, cut off from nourishing blood vessels, are starved of oxygen (hypoxia) and die, becoming necrotic cells (N).
The remaining six equations track angiogenesis (new blood vessel formation), oxygen levels, and rates of necrosis and cell division.
Built for Speed
Fathallah-Shaykh’s first GBM model, published in August 2014 in the Bulletin of Mathematical Biology, consisted of many more equations. It required a supercomputer, and several days, to run. The model published in PLOS ONE can run in 50 seconds on a typical desktop computer.
And They’re Off!
The simulation begins with a tiny clump of tumor cells surrounded by healthy brain. As the program continues over several virtual weeks, this mass expands in the characteristic manner seen on patient MRIs, with a dark region of necrotic cells in the center, surrounded by a large group of proliferative cells and an outer rim of invasive cells.
Grow or Go
The model’s main assumption is that proliferative cells can turn into invasive cells in hypoxic conditions. This is in keeping with the “grow or go” hypothesis of GBM behavior, which says that low oxygen levels spur GBM cells to flee the dying core of the tumor. When these new invasive cells reach healthy, oxygenated areas of brain, they switch back into proliferative mode and start growing again.
How GBM Escapes Anti-Angiogenesis Therapy
As tumors grow, cells at the core lose contact with nourishing blood vessels and die.
To get around this problem, tumors release VEGF (vascular endothelial growth factor), which induces the body to create new blood vessels (a process known as angiogenesis). In fact, the well-known Folkman Hypothesis states that tumors must be able to induce blood vessel growth in order to keep growing.
Clinicians had high hopes that anti-angiogenesis medications such as bevacizumab (Avastin), could keep tumor growth in check. But two high-profile Phase III clinical trials, which released results in early 2014, found that bevacizumab therapy did not prolong overall survival in patients with recurrent GBM, although it did extend progression-free survival and patient quality of life.
Fathallah-Shaykh’s model, programmed to simulate the effects of anti-angiogenesis therapy, reveals an explanation for this “unusual clinical finding.” When bevacizumab therapy causes oxygen levels to drop, proliferative cells turn into invasive cells and flee the scene. When they reach an area with sufficient oxygen, they convert back into proliferative cells and begin a new cycle of growth. This sets up the tumor for rapid “rebound” growth as soon as it becomes resistant to bevacizumab or therapy is discontinued. That explains why patients treated with bevacizumab in the recent trials didn’t experience any increase in overall survival rates over those who were not treated.
Toward New Treatment Approaches
The model underlines the importance of better understanding the molecular mechanisms of brain cell invasion, particularly the active transport of invasive cells toward healthy brain regions, says Fathallah-Shaykh.
There are currently no available biomarkers to identify the quantity of invasive cells in a patient’s tumor. But finding such a biomarker, and drugs that can target these cells to prevent tumor migration, is a current research focus in Fathallah-Shaykh’s lab. “If we’re going to kill these tumors,” he said, “we have to target the cells that are invading.”
Tuesday, December 2, 2014
Creating a roadmap to bring innovative medical technologies to market
Robert Hergenrother, Ph.D., isn’t a surgeon, but he has done some of his best work in the operating room. In his three decades in the medical device industry, Hergenrother has led engineering teams that have created 15 products, including new technologies for use in brain surgery, wound care and diagnosing disease. “When you have a surgeon come up to you and say, ‘If it wasn’t for your device, I couldn’t have helped that patient,’ that’s pretty powerful,” Hergenrother said.
As the director of the new Alliance for Innovative Medical Technologies (AIMTech), Hergenrother is focused on creating the next generation of life-changing medical devices in Birmingham. AIMTech is a partnership between UAB and Southern Research Institute, modeled after the two institutions’ successful Alabama Drug Discovery Alliance. It will identify promising projects already in development at both institutions and launch new projects that meet pressing clinical needs, Hergenrother explains. AIMTech will provide investment and support to bring these projects through clinical trials and FDA approval. Then the devices will be spun off in startup companies or licensed to major medical device makers.
Scouting for the Next Big Thing
Hergenrother, who also has a faculty appointment in the UAB Department of Biomedical Engineering, is now meeting with clinicians and researchers across campus. “In one day I can go from drug delivery to sports medicine to physical therapy to radiology,” he said. “I get to see a lot of different ideas and work with people who really are excited about moving these ideas forward.”UAB Department of Physical Therapy. Others are simply intriguing concepts. Hergenrother recently met with a surgeon who wants to develop a new tool for cartilage repair. “He had an idea and a drawing,” Hergenrother said. “We were able to come in and make a quick prototype and put it in his hands. He was fired up. It’s a great way to just start answering questions: ‘Is this working, yes or no?’”
Conversations with UAB clinicians will lead to opportunities to create entirely new types of devices. “We want to focus on what is causing people problems now,” Hergenrother said. One of his main jobs, he explains, is to connect clinicians with researchers who can develop solutions to meet their needs.
Hergenrother, who holds 18 patents of his own, understands the thrill of a new invention. But creating a successful medical device isn’t a matter of innovation alone, he points out. As part of the initial scouting phase of the program, “I’m asking investigators to work with me to conduct 20 interviews with the people who will be the ultimate end-users of their product,” he said. “They need to find out how people are doing the job now, what the current solutions are and what advantages their product has to offer.”
Competitive Advantages
Major medical device companies are always eager for new ideas, Hergenrother says. As the industry matures — it is projected to grow by nearly 21 percent by 2016 — those companies are focusing more on international expansion and production efficiencies, he adds. “They’re relying on smaller companies and universities to drive innovation.”Top TargetsAIMTech will initially focus on developing projects in five key areas: | |
| Cardiology |  |
| Orthopedics |  |
| Ophthalmology |  |
| Rehabilitation Engineering |  |
| Trauma |  |
In industry jargon, this is known as “de-risking” — building up the scientific and marketing data necessary to justify a major financial investment. AIMTech will be able to supply that proof by tapping into the combined capabilities of Southern Research and UAB.
UAB’s Institute for Innovation and Entrepreneurship (IIE) will vet the intellectual property position of every project that enters the AIMTech program. IIE and Southern Research will also evaluate potential market size, regulatory pathways and reimbursement strategies so that only the strongest, most market-ready technologies advance through AIMTech’s pipeline. Southern Research has extensive experience in assembling product-development systems and negotiating the regulatory requirements of clinical trials and FDA approvals, Hergenrother notes. “Someone has to do that work,” he said. “If we can take our projects further along than another university, ours will be more attractive to potential partners.”
AIMTech’s ultimate mission is to get life-changing products to market as quickly as possible, Hergenrother says. “We always want to keep in mind why we’re doing this. It’s not to get another patent, but to save lives. We have an opportunity to really make a difference here.”